Employee Benefits Market Check Survey: Employer Strategies for GLP-1 Drugs
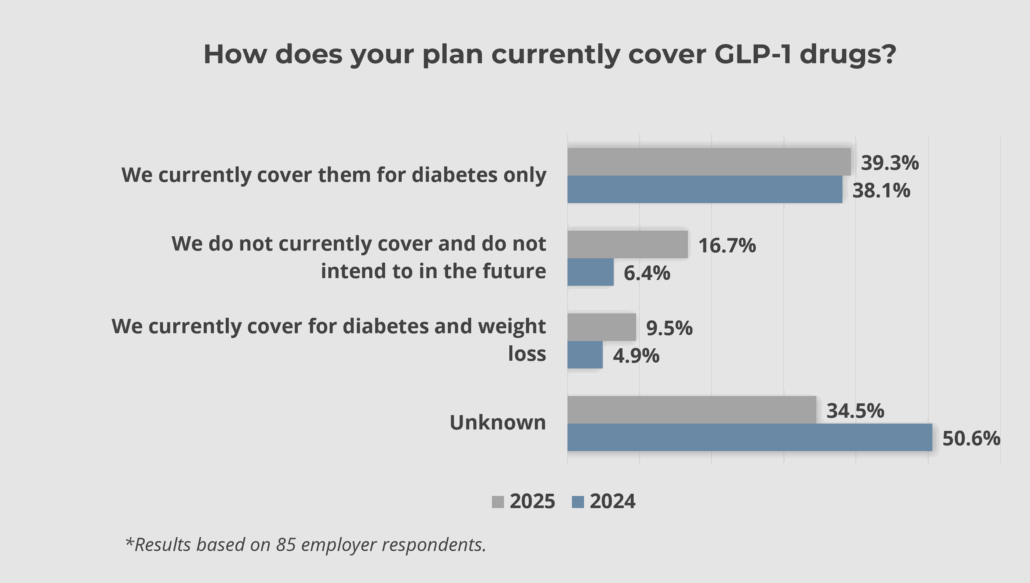
The market for GLP-1 drugs such as Wegovy or Ozempic continues to change quickly. Competition for various forms of these drugs has heated up, and other forms are being developed. Further, these drugs are becoming less invasive, which means interest and demand may be on the rise. While these medications may support improved employee health, the high cost and questions about long-term use present challenges.
To better understand how employers are approaching GLP-1 drug coverage decisions, we conducted a survey on May 22 to explore how coverage has changed since last year and what additional factors are being considered. The results are summarized below.
Key Findings
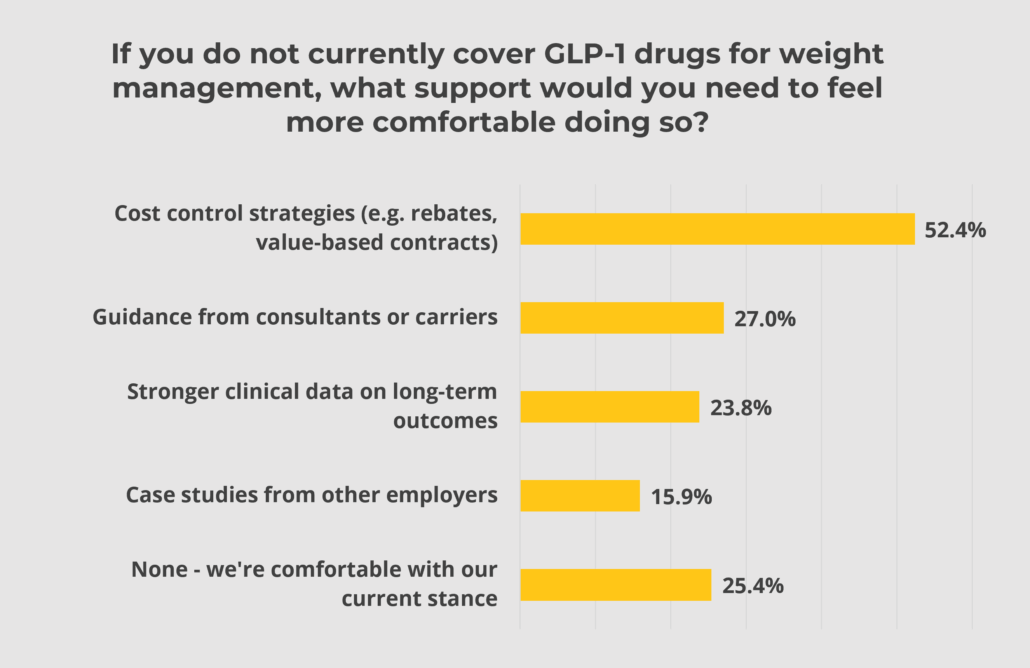
GLP-1 drugs continue to be a difficult subject for employers. These drugs have demonstrated a real impact on an individual’s health; however, the costs continue to rise and can exert enormous pressure on benefit budgets that are already pushed to their limit. Further, the long-term impacts of these drugs have not been studied to any great extent.
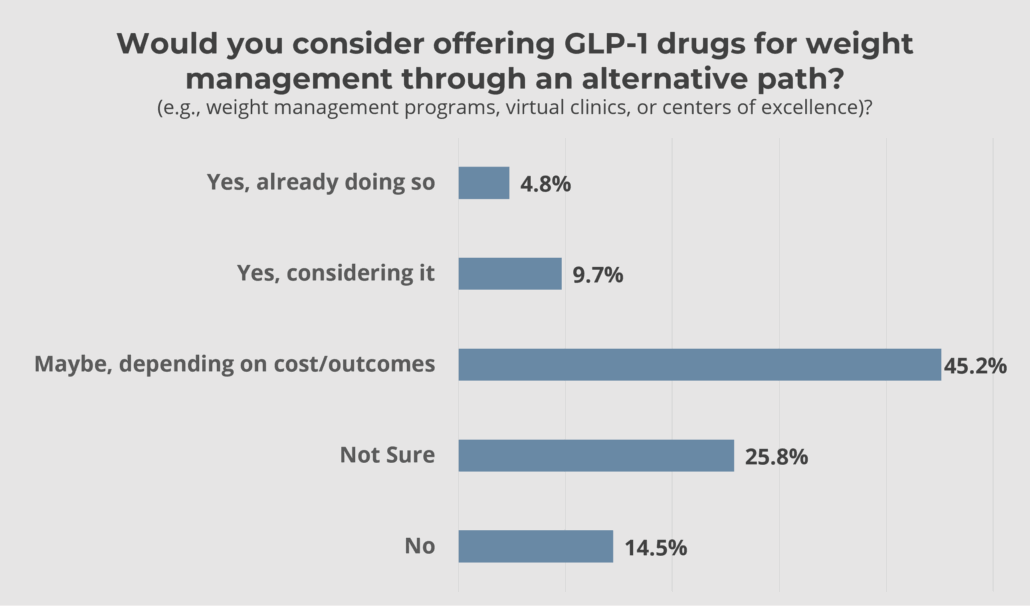
While more employers are covering GLP-1 drugs for weight loss than last year, the vast majority are not, citing cost concerns and clinical uncertainty. Growing employee interest, emerging offerings from insurers and PBMs, and evolving data on long-term outcomes may prompt employers to revisit their strategies. As this landscape continues to shift, we encourage employers to consider a balanced approach. Coverage of these pharmaceuticals should be in conjunction with other wellness and disease management programs.
An established plan will be important for employers exploring coverage of these drugs. Working closely with your benefits broker can help you navigate these considerations and design a strategy that aligns with your organization’s goals and budget.




Leave a Reply
Want to join the discussion?Feel free to contribute!