Assurex Global Market Check Survey: Impacts of HIPAA and Cobra Deadline Suspensions
COVID-19 had great impacts on all parts of business in 2020, and employee benefit plans were no exception. As a result of this pandemic, the
Department of Labor (DOL) put notification periods for HIPAA and COBRA on hold. This means that anyone meeting the appropriate criteria could
enroll in the plan or elect coverage within the outbreak period (defined as 3/1/20 until 60 days after the end of the national emergency). This change
created additional administrative issues, as well as potential financial risk, for group health plan sponsors.
We conducted a poll during a webcast on December 17 to determine what impact has occurred and the results are in the charts below.
Percent of Employers Who Have Had at Least One Late HIPAA Special Enrollment or Late COBRA Election
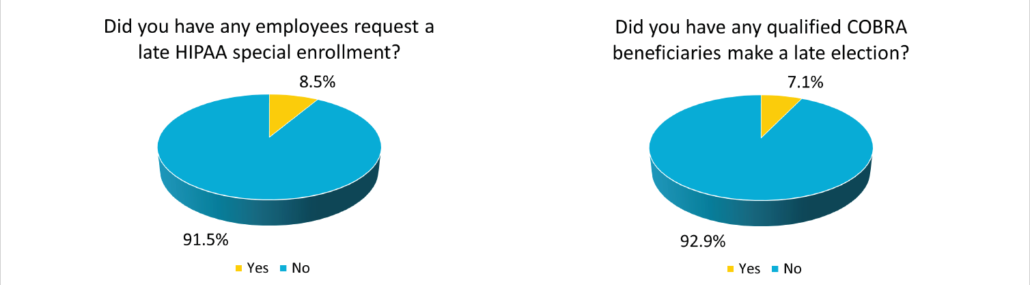
Based on 456 employer respondents; December 17, 2020
While most employers were not adversely affected by the additional time, there remained numerous people that were granted coverage when they
otherwise would have been ineligible. Access to health insurance is always welcome, but employers will have to monitor the financial impacts the
late enrollees might bring.Should you need any assistance with understanding the impact this may have on your population, please contact your local
Assurex Global adviser.
HIPAA – Health Insurance Portability and Accountability Act
COBRA – Consolidated Omnibus Budget Reconciliation Act




Leave a Reply
Want to join the discussion?Feel free to contribute!